Fundamentally Flawed COVID-19 'Science'
The Misinformation That Crushed Constitutional Freedoms Of Healthy/Asymptomatic People
The Vilification of Healthy People; Especially Children
Throughout the past several years apparently healthy people have been re-defined as being potential asymptomatic spreaders of a disease that can be lethal in high-risk individuals. The disease is known as the novel coronavirus disease that was first identified in 2019 (COVID-19). People around the world have been instilled with near-paralyzing fear that their family member, friend, neighbour and/or colleague who has no signs or symptoms can kill them by spreading severe acute respiratory syndrome-coronavirus-2 (SARS-CoV-2), which is the causative agent of COVID-19.
This paradigm that a person has no way of knowing who is safe to be around has formed the rationale for mass lockdowns, masking, and mandating ‘vaccines’ for which the initial clinical experiments are still ongoing. This has caused massive fracturing of relationships around the globe. Nobody has been spared. Families have split, best friendships that lasted decades ended abruptly, and colleagues lashed out.
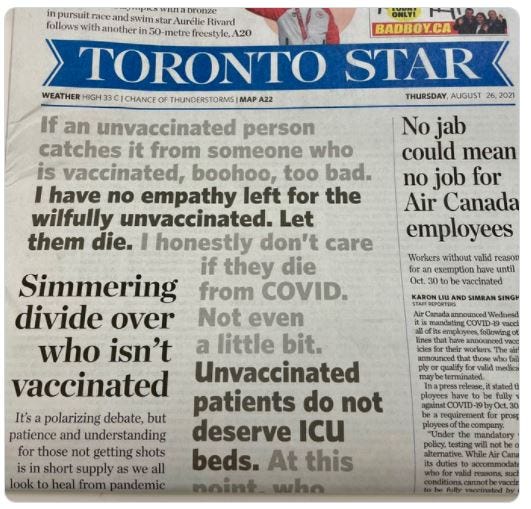
We were told that everyone had to do their part to prevent hospitals from being overwhelmed. Those who felt healthy could not be trusted. Unbeknown to them they might have a wicked pathogen oozing out of their body. Healthy children who were at a statistical risk equivalent to zero of dying from COVID-19 would almost certainly kill their grandparents if they were not locked down, masked and ‘vaccinated’. Those who resisted lockdowns, masking, and mandating of so-called vaccines that could neither prevent the disease nor transmission of its causative agent have been treated like uncaring villains that are deserving of segregation. Remember this front page of one of Canada’s best-known newspapers that was published on August 26, 2021?…
The Prime Minister of Canada, Justin Trudeau, has been a classic example of a leader who has vigorously promoted this kind of hatred and division within his own country.
…EVERYONE AROUND THE WORLD NEEDS TO UNDERSTAND THAT THIS HATRED HAS BEEN DRIVEN BY SCIENTIFIC DATA THAT ARE FATALLY FLAWED AND SNOWBALLING!
So, how did we get so far off-track with our response to COVID-19?
Why will future history books, if accurate, document this as the most mismanaged crisis of our time?
Most of the blame rests on the scientific and medical community allowing a very elegant scientific test to be chronically misused. This test is known as the ‘reverse transcriptase-polymerase chain reaction’ (RT-PCR).
Did we follow the science?
In court, I have often seen judges puzzled by the apparent contradictions in the scientific evidence being put forward by various experts. These judges often question how scientists can interpret the same data so differently. When it comes to the science underpinning COVID-19, published papers can be placed into two bins:
Those that are trustworthy because they are based on sound scientific methods.
Those that are untrustworthy because they are based on flawed scientific methods.
In the past several years science in bin 2 has become voluminous and has contributed excessively to the rationale for the so-called prevailing ‘COVID-19 narrative’. The problem is that the science in bin 2 cannot be properly interpreted because it is built on a fundamentally flawed foundation. Too many scientists failed to critically assess the methods used to generate the early COVID-19 data. This has resulted in this junk science to snowball out of control. The RT-PCR test is at the heart of this problem.
The House Built on Sand Must be Dismantled
If one goes back to the birth of COVID-19 science and critically assesses it, misusing the RT-PCR test jumps out as a key fundamental flaw that caused substantial overestimation of the number of cases of COVID-19 and erroneous labeling of healthy people as asymptomatic spreaders of a deadly disease. The only way to correct course and stop the avalanche of faulty COVID-19 science is to establish which papers can and cannot be trusted. Importantly, editors of scientific journals cannot allow any more COVID-19 ‘facts’ to be published unless the authors unequivocally demonstrate that their data are based on methods that have been implemented properly. Most notably, authors must demonstrate that their research methodologies have been appropriately calibrated such that their conclusions are justified.
Misuse of An Elegant Scientific Technique Has Plagued COVID-19 Science From the Very Beginning
To properly gauge the scope of an outbreak of an infectious disease, one first needs to accurately diagnose it. Diseases are diagnosed primarily based on two things:
Accurately detecting the presence of a pathogen using a laboratory-based test.
Detection of signs and/or symptoms consistent with the disease, which is usually done by a physician.
Symptoms are aspects of a disease that a person experiences but cannot be assessed easily by an observer. Examples include general malaise, pain, and a loss of appetite. In contrast, signs of illness can be objectively observed and documented by others, and include coughing, sneezing, or a fever that can measured with a thermometer. Often, symptoms precede the onset of signs of illness.
When it comes to defining what it means to be ‘asymptomatic’, there are three relevant scenarios:
A person who is not infected with a pathogen will never be at risk of developing the disease associated with that pathogen. These are healthy individuals who are asymptomatic by virtue of not having been infected. They cannot infect others.
A person can be infected with a potential pathogen but never develop symptoms of a disease because the causative agent fails to cause substantial harm in the body. In many cases, this might be because the immune system can respond rapidly and effectively. There have also been examples of people getting infected with SARS-CoV-2 but never apparently experiencing symptoms nor developing signs of COVID-19. Infection does not always result in disease. For example, billions of microbes, including many bacteria and viruses, live on and in our bodies without causing us harm. They have invaded our bodies but do not cause disease, even though some of them can cause serious disease in other people or even ourselves should they get into an inappropriate physiological location (e.g., some fecal bacteria entering a body via the oral route). Infected but asymptomatic (disease-free) people are also healthy (i.e., there is no impairment to their ability to function in their daily activities).
People who get infected and then progress to a diseased state always have a period in between when they are ‘asymptomatic’. Technically, these individuals that do eventually get sick are referred to as being ‘pre-symptomatic’. One does not know if a person is truly asymptomatic or pre-symptomatic until the typical incubation period for a pathogen has passed; this is the expected time from infection to the onset of symptoms in a susceptible person. A person who is infected and symptomatic can spread the causative agent of the disease to others.
When people have COVID-19, they experience obvious symptoms and signs also usually become apparent. This is the scenario that has been easy to manage throughout the declared COVID-19 pandemic. People who are sick have been asked to stay home. From a social hygiene perspective, it is my expert opinion that this should be encouraged for all the infectious diseases we live with. This would reduce infectious disease-related morbidities and mortalities.
In the context of COVID-19, most masking, isolation and vaccination policies around the world are predicated on the assumption that transmission of SARS-CoV-2 can be efficiently mediated by asymptomatic people who are transiently infected but never get COVID-19 and/or pre-symptomatic individuals. This is based on the assumption that SARS-CoV-2 can replicate to the point where a person who is not coughing or sneezing can expel a threshold dose required to potentially infect another person. Although this is theoretically possible and likely occurs rarely, it is incorrect to conclude that this is commonplace and a significant driver of the spread of COVID-19. This incorrect concept is based on an array of scientific studies that relied on RT-PCR testing that was inappropriately calibrated.
How to Define a Case of COVID-19
Cases of COVID-19 should only be determined as follows:
It should be a physician making the diagnosis.
It should be based on the presence of signs and symptoms that are consistent with the clinical definition of COVID-19.
The presence of symptoms and/or signs should be supported by laboratory results derived from properly calibrated tests that demonstrate the presence of SARS-CoV-2 virions. A virion is a single virus particle. Virions can be replication-competent; these are the only ones that can potentially infect another person and cause disease. Or they can be replication-incompetent; these ones can never spread to others and cause COVID-19.
Throughout the declared pandemic many so-called ‘cases’ of COVID-19 were incorrectly ‘diagnosed’. Cases, especially early in the declared pandemic, have been defined by individuals other than physicians, assumed based on signs and symptoms only, or exclusively based on a positive laboratory test result. The latter has been extremely common. This contradicts the World Health Organization, which noted that “Most PCR assays are indicated as an aid for diagnosis, therefore, health care providers must consider any result in combination with timing of sampling, specimen type, assay specifics, clinical observations, patient history, confirmed status of any contacts, and epidemiological information”.
The core definition, and all-too-often the sole definition of ‘cases’ of COVID-19 has been based on the use of a laboratory testing method referred to as ‘RT-PCR’. To understand how asymptomatic people were mislabeled as significant sources of transmission of SARS-CoV-2, one must first understand how RT-PCR testing should have been properly calibrated around the world.
A polymerase is a protein that can copy DNA, which is a genetic blueprint. So, the PCR method requires this genetic blueprint known as DNA to be present in order to work. If DNA is in a sample, when a scientist adds a polymerase, a few other ingredients, and then varies the temperature, new copies of tiny portions of the DNA will be made. With each ‘cycle’ that the PCR test is run, more copies of these fragments of the genetic blueprint will be made. Once a threshold number of copies appear in the sample, they can be detected. Think of it like a photocopier. From a great distance, you might not be able to tell if a single copy of a page has been made. However, once you have a stack of five hundred pages sitting on the output tray, you know for sure that the photocopier is churning out copies. In short, PCR is a method that scientists can use to determine whether a particular genetic blueprint is present in a sample.
The genetic blueprint for SARS-CoV-2 is not made of DNA. Instead, it is made of a related structure called ‘RNA’. Therefore, to use the PCR test to determine whether an RNA-based virus is present in a sample requires one additional step at the beginning. Specifically, a ‘reverse transcriptase’ is used to convert the RNA from SARS-CoV-2 into DNA, portions of which can then be detected with the PCR test. This is how the RT-PCR test is used to detect the presence of small pieces of the genetic material from SARS-CoV-2.
The Inappropriate Use of RT-PCR Testing Caused a Disconnect Between Laboratory Studies and ‘Real World’ Data
Laboratory studies suggested that asymptomatic individuals could potentially shed infectious SARS-CoV-2 one to two days before the onset of symptoms of COVID-19. However, the largest ‘real world’ study done to date looked at the prevalence of SARS-CoV-2 in ~10 million people in Wuhan, China and found no evidence of asymptomatic transmission. This typical disconnect in the results of laboratory-based studies and ‘real world’ data is due to the former types of experiments having relied on the use of uncalibrated or incorrectly calibrated RT-PCR tests. An RT-PCR test can only determine if tiny fragments of the genetic material from a virus is present in a sample. It can never indicate, on its own, whether that material is from virus particles that have the potential to infect and cause disease, or from replication-incompetent virions or even portions thereof that cannot cause disease.
Flawed RT-PCR Testing Caused Over-Diagnosis of COVID-19
On its own, a positive result on a RT-PCR test to detect SARS-CoV-2 is insufficient to diagnose COVID-19, yet this became routine in most parts of the world. In addition to the potential for false positive tests, true positive results can also be obtained from genomes of SARS-CoV-2 particles that are no longer infectious. An example of the latter would be an individual who has mounted an effective immune response and may have remnant replication-incompetent viral particles or partially degraded viral genetic material inside relatively long-lived white blood cells that have killed the virus. These cells are known as ‘phagocytes’ and are part of our immune system. Indeed, following clearance of SARS-CoV-2 from the body, full and/or partial genomes of SARS-CoV-2 can remain for up to several weeks. Phagocytosis (or ‘eating’) of SARS-CoV-2 is a mechanism to kill and remove the virus from the body. These phagocytic cells tend to hang on to these ‘killed’ virions so that they can activate other immunological effector cells, including B cells that produce the antibodies we have heard so much about. As such, these phagocytes can be a source of SARS-CoV-2 genomes that could be amplified by a PCR test. However, these genomes would not have the potential to cause COVID-19. Instead it would evidence that the infection has resolved or is resolving. Persistence of whole or partial genomes that are not associated with infectious particles is well-documented for a variety of other viruses, including measles, Middle East respiratory syndrome-coronavirus, and other coronaviruses. A positive RT-PCR test for the presence of SARS-CoV-2 should never be used, on its own, to define cases of COVID-19; and definitely should not be used to claim that someone has the potential to infect another person.
Building a Rock-Solid Foundation for COVID-19 Science:
The Gold Standard Functional Virology Assay that Should Always be Used to Calibrate RT-PCR Tests
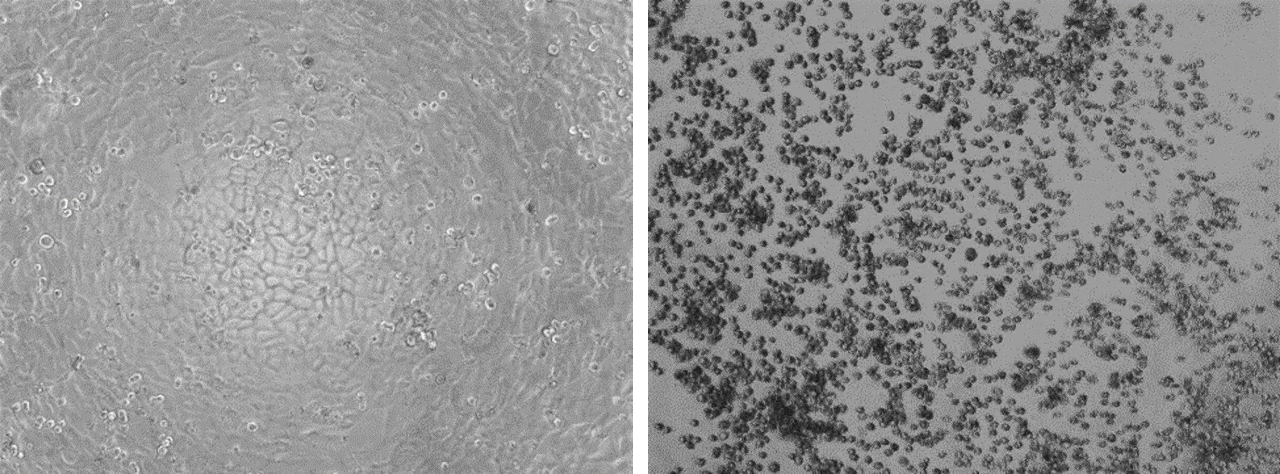
A gold standard test for infectivity of a virus is a cell-based functional assay that determines the potential to replicate and cause cell death. The assay works like this: Cells that are stripped of their anti-viral properties are put into a dish and allowed to adhere to the bottom. The cells would typically cover the entire bottom of the dish. A scientist can look under a microscope to confirm the cells are healthy. A sample then gets added to the cells. If the sample contains replication-competent (i.e., potentially disease-causing) virions, these will infect and kill the cells. A day or two later, the scientist can check the cells under a microscope again. If they see what is called a ‘cytopathic effect’, which means the cells have died, this indicates that replication-competent virions were present. If there was no cytopathic effect, there were no replication-competent virions. Here are pictures from my research team that show how this virology test works…
…the cells on the left were not exposed to a replication-competent (infectious) virus. They remain happily adhered to the bottom of the dish. There was no cytopathic effect. The cells on the right were exposed to a replication-competent virus that infected and killed them. As the cells died, they rounded up and lost their ability to remain stuck to the bottom of the plate. This is a classic example of cytopathic effect. You can see how easy it is to use this test to determine whether a sample contains any infectious virions.
To calibrate a RT-PCR test for SARS-Cov-2, samples from nasopharyngeal swabs of a large array of people would be split into two; one for RT-PCR testing and the other for testing in the gold standard virology assay. Scientists would note the cycle threshold values from the RT-PCR test that are associated with evidence of replication-competent virions from the cellular virology assay versus those that did not cause a cytopathic effect. This allows a cycle threshold cut-off to be determined. Above this threshold, there is no evidence of replication-competent virions in samples from the nasopharyngeal swabs. This is the objective and proper way to calibrate a RT-PCR test when studying transmission of a virus. Without doing this, RT-PCR test results cannot be interpreted in a meaningful way, and they would lead to inappropriate conclusions, like asymptomatic people being spreaders of COVID-19.
Early in the declared COVID-19 pandemic the Public Health Agency of Canada appropriately performed this calibration of their RT-PCR test. For the test they were using, they identified a cycle threshold cut-off of 24 for declaring people to have the potential to infect others. If they had subsequently offered this service to support studies of the spread of COVID-19, only samples yielding a signal at 24 or fewer cycles would be declared to have evidence of potentially infectious SARS-CoV-2. However, with no explanation provided, this initial and appropriate way of calibrating the RT-PCR assay was not required for labs around the world that were studying transmission of SARS-CoV-2. In fact, cycle threshold cut-offs were arbitrarily assigned. As such, RT-PCR data used to determine global cases of COVID-19 have been highly unreliable.
Even so-called ‘fact-checkers’ of people who criticized the inappropriate designation of the RT-PCR as a stand-alone gold standard diagnostic test have had to admit that it cannot possibly distinguish between infectious and non-infectious virions or parts thereof. For example, a ‘fact check’ from Reuters concluded “PCR tests are being used widely in England to show that SARS-CoV-2 viral genetic material is present in the patient”. I bolded the relevant text. Indeed, RT-PCR tests are a valuable tool for determining whether portions of a virus’s genetic material are present in a sample. They cannot determine whether that genetic material is from a replication-competent virion that would have the potential to infect someone.
Positive RT-PCR tests for SARS-CoV-2 in asymptomatic people are almost universally based on high cycle threshold values, which raises the question of whether these individuals harbor infectious viral particles. The absence of a functional cell-based assay to prove infectivity renders results of asymptomatic testing impossible to interpret accurately. Indeed, the World Health Organization, agreeing with many health professionals around the world, has emphasized that spreading of SARS-CoV-2 by asymptomatic individuals is rare and an emphasis should be placed, therefore, on testing people with signs or symptoms of illness, not those who are apparently healthy.
In addition to the Canadian study that identified a cycle threshold of 24 as an appropriate cut-off for declaring samples positive for infectious SARS-CoV-2, other studies reported results of similar calibrations of other RT-PCR assays for SARS-CoV-2. They identified cycle threshold cut-offs of 22-27 and 30. Altogether, this suggests that tests with cycle threshold values above 22-30 are likely not indicative of the presence of replication-competent SARS-CoV-2.
The logical conclusion is that it is erroneous to declare samples with high cycle threshold values, especially those above 30, as being positive for infectious SARS-CoV-2. However, in many countries people were assumed to be infectious when their samples were declared positive using RT-PCR assays with cycle threshold cut-offs as high as 45 cycles. Such an unjustifiably high cut-off would have resulted in a substantial overestimation of cases of COVID-19 and would have led to erroneous labeling of asymptomatic people as potential spreaders of COVID-19.
Failure to Calibrate the RT-PCR Test Shows How a Representative Influential Scientific Study Incorrectly Concluded that Asymptomatic People Might be a Risk for Spreading COVID-19
The figure below shows results of a published study that claimed to depict the frequency at which asymptomatic people tested positive for SARS-CoV-2 relative to that observed for people with symptomatic infections. Specifically, graphs are shown from figure 2 of a paper published in the influential Journal of the American Medical Association - Internal Medicine. The argument being made was that the frequency at which asymptomatic people tested positive for SARS-CoV-2 was like that observed for people with symptomatic infections. However, the authors failed to calibrate their RT-PCR assay.
Following is the description the authors of the study provided in the methods section of their paper. The most important portion of this text is the last sentence, which is bolded.
“Specimen Collection and RT-PCR for SARS-CoV-2
The URT specimens were collected from both nasopharyngeal and oropharyngeal swabs obtained by trained medical staffs (physicians and nurses). For LRT specimens, participants were given instructions the night before to collect a first morning sputum (after gargling) in a specimen cup; RT-PCR assays for SARS-CoV-2 were performed using Allplex 2020-nCoV assay (Seegene, Seoul, ROK) to determine the presence of virus through the identification of 3 genetic markers: envelope (env) gene, RNA-dependent RNA polymerase (RdRp) gene, and nucleocapsid protein (N) gene. The cycle threshold (Ct) during RT-PCR testing refers to when the detection of viral amplicons occurs, it is inversely correlated with the amount of RNA present. A lower Ct value indicates large quantities of viral RNA. It was considered positive when the Ct values of all genes were less than 40 cycles.”
Remarkably, the authors applied an arbitrary cycle threshold of 40 to define a positive test result. Proper calibration of the test was not performed. I applied a new cycle threshold cut-off of 24, based on the published results of the Canadian study for calibrating a RT-PCR test for SARS-CoV-2. This is shown as a red dotted line on the graphs in the figure above. Symbols appearing in the light red rectangle above this line would be considered negative, in contrast to the positive designation that the authors had assigned. Remarkably, 99.7% of the people the authors declared to be harbouring infectious SARS-CoV-2 likely had no evidence of potentially infectious SARS-CoV-2 virions, had the test been properly calibrated. This represents a fatal flaw in this paper; one that negates its conclusion that “Isolation of asymptomatic patients may be necessary to control the spread of SARS-CoV-2”. It should also precipitate its retraction. Such a paper should never have been allowed to be published in the first place.
This highlights a fatal flaw that has been extremely common in publications throughout the declared pandemic that claimed asymptomatic people could be a significant source of transmission of SARS-CoV-2 that could cause COVID-19 in other people. Every paper making this claim should have the materials and methods section carefully evaluated to determine whether the cycle threshold cut-off for the RT-PCR assay was based on the appropriate calibration method or was selected arbitrarily.
Here is a list of other influential publications of original research studies that erroneously concluded that asymptomatic people might be significant sources of replication-competent SARS-CoV-2 virions. Most are based on fatally flawed RT-PCR testing and the remaining papers fail to disclose how they defined an ‘infection’. All of them should be retracted. None of their conclusions can be trusted…
Bai, Y. et al. Presumed Asymptomatic Carrier Transmission of COVID-19. Jama 323, 1406-1407 (2020).
Arons, M.M. et al. Presymptomatic SARS-CoV-2 Infections and Transmission in a Skilled Nursing Facility. The New England journal of medicine 382, 2081-2090 (2020).
Stock, A.D. et al. COVID-19 Infection Among Healthcare Workers: Serological Findings Supporting Routine Testing. Front Med (Lausanne) 7, 471 (2020).
Bi, Q. et al. Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. The Lancet. Infectious diseases 20, 911-919 (2020).
Böhmer, M.M. et al. Investigation of a COVID-19 outbreak in Germany resulting from a single travel-associated primary case: a case series. The Lancet. Infectious diseases 20, 920-928 (2020).
Chan, J.F. et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (London, England) 395, 514-523 (2020).
Van Vinh Chau, N. et al. The Natural History and Transmission Potential of Asymptomatic Severe Acute Respiratory Syndrome Coronavirus 2 Infection. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 71, 2679-2687 (2020).
Chaw, L. et al. Analysis of SARS-CoV-2 Transmission in Different Settings, Brunei. Emerging infectious diseases 26, 2598-2606 (2020).
Cheng, H.Y. et al. Contact Tracing Assessment of COVID-19 Transmission Dynamics in Taiwan and Risk at Different Exposure Periods Before and After Symptom Onset. JAMA internal medicine 180, 1156-1163 (2020).
Gao, M. et al. A study on infectivity of asymptomatic SARS-CoV-2 carriers. Respiratory medicine 169, 106026 (2020).
Gao, Y. et al. A cluster of the Corona Virus Disease 2019 caused by incubation period transmission in Wuxi, China. The Journal of infection 80, 666-670 (2020).
Guan, W.J. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. The New England journal of medicine 382, 1708-1720 (2020).
He, X. et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 26, 672-675 (2020).
Hodcroft, E.B. Preliminary case report on the SARS-CoV-2 cluster in the UK, France, and Spain. Swiss medical weekly 150 (2020).
Hoehl, S. et al. Evidence of SARS-CoV-2 Infection in Returning Travelers from Wuhan, China. The New England journal of medicine 382, 1278-1280 (2020).
Lauer, S.A. et al. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Annals of internal medicine 172, 577-582 (2020).
Li, R. et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science (New York, N.Y.) 368, 489-493 (2020).
Li, C. et al. Asymptomatic and Human-to-Human Transmission of SARS-CoV-2 in a 2-Family Cluster, Xuzhou, China. Emerging infectious diseases 26, 1626-1628 (2020).
Liu, Y., Funk, S. & Flasche, S. The contribution of pre-symptomatic infection to the transmission dynamics of COVID-2019. Wellcome open research 5, 58 (2020).
Lu, X. et al. SARS-CoV-2 Infection in Children. The New England journal of medicine 382, 1663-1665 (2020).
Lu, S. et al. Alert for non-respiratory symptoms of coronavirus disease 2019 patients in epidemic period: A case report of familial cluster with three asymptomatic COVID-19 patients. Journal of medical virology 93, 518-521 (2021).
Luo, S.H. et al. A confirmed asymptomatic carrier of 2019 novel coronavirus. Chinese medical journal 133, 1123-1125 (2020).
Mizumoto, K., Kagaya, K., Zarebski, A. & Chowell, G. Estimating the asymptomatic proportion of coronavirus disease 2019 (COVID-19) cases on board the Diamond Princess cruise ship, Yokohama, Japan, 2020. Euro surveillance : bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin 25 (2020).
Sun, K. et al. Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. Science (New York, N.Y.) 371 (2021).
Nishiura, H. et al. Estimation of the asymptomatic ratio of novel coronavirus infections (COVID-19). Int J Infect Dis 94, 154-155 (2020).
Nishiura, H., Linton, N.M. & Akhmetzhanov, A.R. Serial interval of novel coronavirus (COVID-19) infections. Int J Infect Dis 93, 284-286 (2020).
Pan, Y., Zhang, D., Yang, P., Poon, L.L.M. & Wang, Q. Viral load of SARS-CoV-2 in clinical samples. The Lancet. Infectious diseases 20, 411-412 (2020).
Pan, X. et al. Asymptomatic cases in a family cluster with SARS-CoV-2 infection. The Lancet. Infectious diseases 20, 410-411 (2020).
Park, S.Y. et al. Coronavirus Disease Outbreak in Call Center, South Korea. Emerging infectious diseases 26, 1666-1670 (2020).
Payne, D.C. et al. SARS-CoV-2 Infections and Serologic Responses from a Sample of U.S. Navy Service Members - USS Theodore Roosevelt, April 2020. MMWR. Morbidity and mortality weekly report 69, 714-721 (2020).
Kimball, A. et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020. MMWR. Morbidity and mortality weekly report 69, 377-381 (2020).
Qian, G. et al. COVID-19 Transmission Within a Family Cluster by Presymptomatic Carriers in China. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 71, 861-862 (2020).
Ran, L. et al. Risk Factors of Healthcare Workers With Coronavirus Disease 2019: A Retrospective Cohort Study in a Designated Hospital of Wuhan in China. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 71, 2218-2221 (2020).
Rosenberg, E.S. et al. COVID-19 Testing, Epidemic Features, Hospital Outcomes, and Household Prevalence, New York State-March 2020. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America 71, 1953-1959 (2020).
Sakurai, A. et al. Natural History of Asymptomatic SARS-CoV-2 Infection. The New England journal of medicine 383, 885-886 (2020).
Samsami, M., Zebarjadi Bagherpour, J., Nematihonar, B. & Tahmasbi, H. COVID-19 Pneumonia in Asymptomatic Trauma Patients; Report of 8 Cases. Archives of academic emergency medicine 8, e46 (2020).
Tabata, S. et al. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. The Lancet. Infectious diseases 20, 1043-1050 (2020).
Tong, Z.D. et al. Potential Presymptomatic Transmission of SARS-CoV-2, Zhejiang Province, China, 2020. Emerging infectious diseases 26, 1052-1054 (2020).
Treibel, T.A. et al. COVID-19: PCR screening of asymptomatic health-care workers at London hospital. Lancet (London, England) 395, 1608-1610 (2020).
Wei, W.E. et al. Presymptomatic Transmission of SARS-CoV-2 - Singapore, January 23-March 16, 2020. MMWR. Morbidity and mortality weekly report 69, 411-415 (2020).
Xu, J., Li, Y., Gan, F., Du, Y. & Yao, Y. Salivary Glands: Potential Reservoirs for COVID-19 Asymptomatic Infection. Journal of dental research 99, 989 (2020).
Yang, R., Gui, X. & Xiong, Y. Comparison of Clinical Characteristics of Patients with Asymptomatic vs Symptomatic Coronavirus Disease 2019 in Wuhan, China. JAMA network open 3, e2010182 (2020).
Yang, N. et al. In-flight transmission cluster of COVID-19: a retrospective case series. Infectious diseases (London, England) 52, 891-901 (2020).
Ye, F. et al. Delivery of infection from asymptomatic carriers of COVID-19 in a familial cluster. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases 94, 133-138 (2020).
Yu, P., Zhu, J., Zhang, Z. & Han, Y. A Familial Cluster of Infection Associated With the 2019 Novel Coronavirus Indicating Possible Person-to-Person Transmission During the Incubation Period. The Journal of infectious diseases 221, 1757-1761 (2020).
Zhang, J., Tian, S., Lou, J. & Chen, Y. Familial cluster of COVID-19 infection from an asymptomatic. Critical care (London, England) 24, 119 (2020).
Almadhi, M.A. et al. The high prevalence of asymptomatic SARS-CoV-2 infection reveals the silent spread of COVID-19. International journal of infectious diseases : IJID : official publication of the International Society for Infectious Diseases 105, 656-661 (2021).
Choi, A. et al. Symptomatic and Asymptomatic Transmission of SARS-CoV-2 in K-12 Schools, British Columbia, Canada April to June 2021. Microbiology spectrum, e0062222 (2022).
…these 48 papers represent most, if not all, of the peer-reviewed scientific evidence that has been used by most public health officials to mislabel asymptomatic people as sources of COVID-19-causing SARS-CoV-2. All of it is fatally flawed.
It was even concluded in a study that patients testing ‘positive’ with cycle threshold values above 33 could likely be discharged from hospitals. Such a recommendation would never be made if there was any evidence that these people harboured SARS-CoV-2 virions with the potential to infect others. So one must wonder why testing labs were allowed to arbitrarily pick cycle thresholds ranging from 38 to 45 as upper limits for defining the presence of infectious SARS-CoV-2.
Exclusive reliance on improperly calibrated RT-PCR testing as an indication of ‘infection’ has also led to the erroneous conclusion that post-symptomatic people may also need to be masked and/or isolated.
I have yet to see appropriate scientific evidence to justify the unusually high cycle threshold values being used in studies that label people as asymptomatic sources of COVID-19. In the absence of such data, there is no justification for masking, isolating or mandating experimental vaccine technologies for asymptomatic people.
Others have also criticized the exclusive use of RT-PCR tests in diagnosing COVID-19 and drawing conclusions about transmission in the absence of infectivity testing.
How RT-PCR Testing Should Have Been Used to Support Diagnoses of COVID-19
All labs should have been required to calibrate their RT-PCR test prior to providing any ‘real world’ data to public health officials that would be used to study the transmission of SARS-CoV-2. Use of the gold standard functional virology assay to do this calibration would have provided each lab with a strong objective rationale for their specific cycle threshold cut-off value when determining whether a person could have the potential to infect others. And this should have always been married to a clinical diagnosis rendered by a physician. As mentioned earlier, if this standard is applied retroactively to the COVID-19 scientific literature, it becomes obvious that much of it is untrustworthy.
Much of the Foundational COVID-19 Science is Fundamentally Flawed
RT-PCR testing has generally been misused during the declared COVID-19 pandemic due to failures to calibrate it properly. The result has been mislabeling asymptomatic people as significant potential sources for transmission of COVID-19. This, in turn, has resulted in inappropriate mandating of masking, isolation, and ‘vaccines’ for people who do not represent a genuine health risk to others. It has also taken the diagnostic expertise away from physicians and placed it in the hands of anonymous laboratory technicians.
Now, we are left with a mountain of COVID-19 science that cannot be interpreted properly. Scientists with integrity and the relevant expertise know that a substantial but undefined number of people that tested ‘positive for COVID-19’ never had the potential to spread SARS-CoV-2 to others and many of these also did not actually have the disease known as COVID-19.
Resolving the Apparent Conflicts in Evidence Presented by ‘Experts’
To judges who are puzzled by the differing interpretations of experts in their courts, the explanation is fairly simple. If you remove the fundamentally flawed science from expert reports, you will be left with trustworthy data that generally do not support what has been the prevailing narrative over the past several years. When scientists talk about following the overall weight of the scientific evidence, what we really mean is to follow the weight of the trustworthy scientific evidence. Do not get bedazzled by the numerous reports that have accumulated, often in ‘prestigious’ journals, that were based on flawed scientific methods. Don’t get distracted by the number of health ‘authorities’ that have blindly propagated this flawed science. Truth is not a democracy. It is not defined by a majority vote.
Harm to Public Trust in Science
The global propagation of poorly conducted science over the past several years has caused massive and irreparable harm. Children and teenagers took the brunt of this damage. They were given no choice. They had no voice. They became shields used in a conflict waged by adults who wielded faulty science like it was the gospel truth.
As a scientist with deep expertise in viral immunology, I am incredibly disheartened by the state of my scientific disciplines. My colleagues that sat in their ivory towers allowing junk science to justify crushing constitutional freedoms should be ashamed of themselves. I am proud of the relatively few who stood tall on a foundation of integrity and endured brutal treatment for the past couple of years. I can only hope that the harm done to public trust in the health sciences can be remedied.





Covid is not an epidemiological story. Covid is a crime story.
If you view this whole 'pandemic' situation through the lens of health, safety, science and saving lives, then most of it makes little sense. If you view it through the lens of money, power, control, and wealth transfer, then all of it makes perfect sense. The official narrative of "Covid" is a fiction- all of it. It is an intelligence operation meant to provide cover for the controlled demolition of the insolvent Western economies.
There was no pandemic- EVER.
This is so clearly articulated!! It's very refreshing to see a masterpiece like this that elegantly, clearly and decisively presents an unrebuttable case for a specific proposition, especially one so fundamental to the pandemic policy voodoo adventurism.
The list of studies that are fatally compromised by their incorporation of the flawed assumption of infectiousness from PCR positive results at a higher CT that can be plausibly presumed to represent infectious/active infection was a really nice touch.
Thanks for taking the time to write this up :)